Maria Paula Ramalho Bajanca-Lavado
National Institute of Health, Portugal
Title: Ampicillin resistance mechanisms in clinical Haemophilus influenzae
Biography
Biography: Maria Paula Ramalho Bajanca-Lavado
Abstract
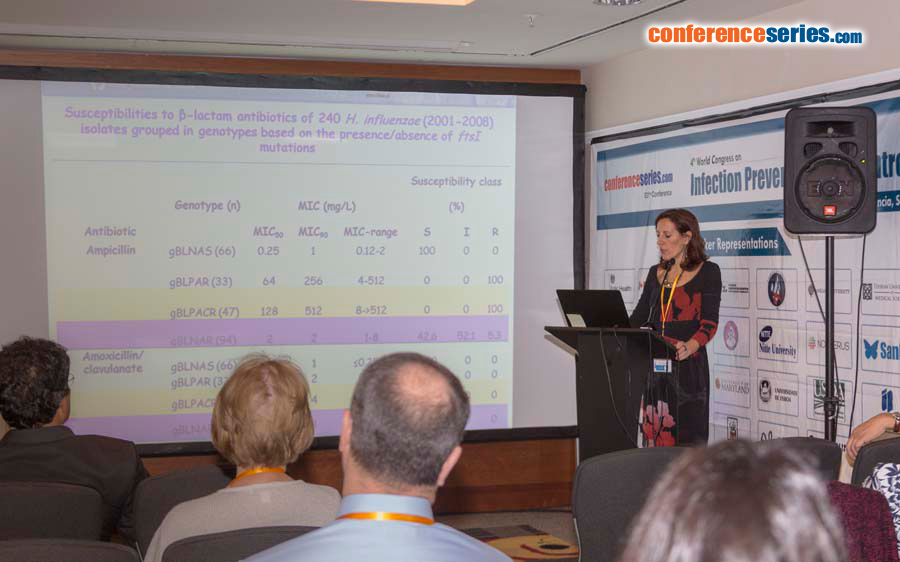
Haemophilus influenzae remains a key etiological agent of upper and lower respiratory tract infections. Two major mechanisms are involved in ampicillin (AMP) resistance: β-lactam hydrolysis due to β-lactamase production (TEM-1 or ROB-1) and decreased affinity of penicillin-binding protein 3 (PBP3) for β-lactam antibiotics as a result of ftsI gene mutations encoding PBP3. Isolates exhibiting this latter resistant mechanism are termed β-lactamase-non-producing ampicillin-resistant (BLNAR), while isolates with both resistant mechanisms are defined as β-lactamase-positive amoxicillin-clavulanic acid-resistant (BLPACR). A variety of amino acid (AA) substitutions within the transpeptidase domain of PBP3 are mainly responsible for resistance. According to specific substitutions, these isolates have been classified in one of three mutational groups: I-III. Group II was further divided into subgroups IIa-IId. More recently, a new group was described, “III-like” with additionally AA substitutions to the ones described in group III. Decreased ampicillin susceptibility have been associated to group I and II, while group III is normally associated with high resistance levels to ampicillin. Isolates with the non-enzymatic resistance mechanisms have been described and emerging worldwide. In this context, we aimed to characterize ampicillin resistance mechanisms in clinical H. influenzae strains isolated in Portugal. Amplification and sequencing of ftsI gene was performed in 568 clinical H. influenza isolates. Analysis of mutations characterized 61% of isolates as gBLNAR or gBLPACR. Most of the strains were included in group II (85%) with predominance of IIb (61%). Rare isolates were of group I and no isolate was classified in group III, although few strains were of group III-like. Our results are indicative of wide dissemination of a non-enzymatic resistance mechanism to β-lactams among H. influenzae isolates circulating in our country, probably due to inappropriate use of oral antibiotics, which is a matter of concern. A better understanding of this issue may help to establish adequate therapeutic and preventive measures to avoid selection or dissemination of such strains.
Speaker Presentations
Speaker PPTs Click Here